To Conserve the Fighting Strength
Placing Medical Assets Closer to the Fight
By COL Patricia Brown
Article published on: November 5, 2024 in the November 2024 Issue of the Pulse of Army Medicine Journal
Read Time: < 15 mins

The accumulation of casualties within any combat unit restricts its movements and lack of proper facilities for the care of the wounded has always exerted a serious depressing effect upon soldiers.
—FM 8-10, Medical Field Manual, 1942
After more than 20 years of war in Afghanistan and Iraq, the people of the United States and the U.S. military grew accustomed to low casualty rates. During that time, 52,036 service members were wounded and 4,986 killed in action, a fatality rate of less than 10 percent.1 This high survival rate occurred when the U.S. and its allies operated out of fixed forward operating bases, with air superiority and medevac assets readily available to take patients from the point of injury (POI) to an operating room within 60 minutes.2 The U.S. will not be so lucky in the event of large-scale combat operations (LSCO) against a near-peer adversary such as China. During Warfighter exercises simulating LSCO against a near-peer, a force of 100,000 sustained between 50,000 to 55,000 thousand casualties, 10,000 to 15,000 of those killed in action, in just eight days.3 This is a fatality rate of 20 to 30 percent, more than double that of the wars in Iraq and Afghanistan. A recent study wargaming a conflict with China over Taiwan calculated that the U.S. forces would sustain 140 killed in action (KIA) daily.4 At that rate, in six weeks, the number of U.S. KIA would exceed the total casualties sustained in Afghanistan and Iraq during the Global War on Terrorism (GWOT).
Not since World War II has the U.S. seen such high casualty numbers. At that time, in the Pacific theater, the first 21 days of the Battle for Iwo Jima saw more than 1,000 casualties daily.5 In just over one month, 20,950 were wounded, and 4,893 lay dead.6 Such high casualty numbers are unfathomable today but may be the reality in the event of another war in the Pacific. The last 20 years of war involved brigade and smaller-sized engagements, with medical assets safely ensconced behind tall walls of concrete and sand. A future fight against a near-peer like China will be one of movement and maneuver. Combat units will constantly move, setting up and breaking down every few hours to survive.7 Combat formations encumbered by casualties cannot effectively maneuver to survive, exploit the initiative, and defeat the enemy. High casualty numbers mean aid stations assigned to support maneuver units will be rapidly overwhelmed. To continue maneuvering to support those units, aid stations must quickly evacuate their casualties to the next level of care.8 Evacuation to definitive care in the Indo-Pacific region during LSCO will be challenging because of the sheer number of casualties, rugged terrain, and lack of sufficient aeromedical assets to meet the need. Consequently, the 60-minute evacuation times that helped reduce the casualty rate during the GWOT may be untenable.9 Prolonged evacuation may be the new norm.
To overcome these challenges, U.S. medical planners must rethink how medical assets are allocated to care for casualties and maintain combat power. Properly configured and placed medical facilities can overcome time and distance constraints to evacuate and treat casualties during LSCO in the Pacific. However, an obstacle to this care is the variability in medical facility configuration between the services.
The treatment capabilities of U.S. military facilities vary based on size, equipment, and personnel. The most basic level is Role 1, which consists of POI care, such as buddy aid and self-aid, and casualty stabilization at a Battalion Aid Station (BAS). At a BAS, medics, a physician, and a physician assistant stabilize casualties so they can be safely evacuated for further care or return to duty with their units.10 The next level, Role 2 care, adds lab functions, dental, x-ray, more advanced trauma stabilization, and patient hold.11 This level of care is typically located in the brigade area with maneuver units. Role 3 care is the highest level of care within a combat theater and provides advanced surgical care, imaging capabilities such as computed tomography, and hospital care.12 This level of care is typically located in the division or corps area, and the distances between these facilities and the POI may be significant.13 Role 2 facilities help fill this gap.
"Prolonged evacuation may be the new norm."
However, while Role 2 facilities increase the level of care for casualties, the current U.S. medical doctrine does not call for the consistent placement of surgical teams within these facilities. In preparation for LSCO in the Pacific, the U.S. Indo-Pacific Command (USINDOPACOM) commander should adopt a policy requiring the placement of Role 2 medical facilities with surgical and patient hold capabilities in the brigade area near the forward line of troops (FLOT). Adopting this policy will facilitate maneuver, rapid evacuation of casualties to save lives with early surgical intervention, and regenerate combat power by returning many to duty within three days.
Clear the Battlefield
One of the critical tasks for medical units is clearing the battlefield of casualties to allow the combat commander freedom of maneuver.14 The Indo-Pacific theater will present challenges to casualty evacuation beyond what would otherwise be expected during LSCO. The jungle terrain, widely dispersed island chains, and long sea lines of communication (SLOC) will make casualty evacuation difficult. Air superiority will not be guaranteed; prolonged evacuation times to Role 3 care will be the norm. Great Britain (GBR) faced similar difficulties in casualty care and evacuation during the Falklands War with Argentina in 1982. The war, fought over a series of islands off the Argentinian coast, was waged more than 8, 000 miles from Britain.15 Most fighting occurred on the two main islands and consisted of rugged terrain with few roads, making ground evacuation difficult.16 Initial damage control surgery was performed on the islands near the fighting, and a patient-holding section held patients until they could be evacuated to Role 3, which was only available on offshore hospital ships.17 Casualty evacuation to these ships sometimes took as long as 36 hours and required transport with helicopters, which was made more difficult by the contested airspace.18,19 Evacuating the wounded in the Pacific during WW2 created similar challenges for U.S. forces. Ground and SLOC were contested, hospital ships were in short supply, transport to them was lacking, and they were frequently anchored far from shore to keep them safe from attack.20 During the invasion of Guadalcanal, evacuating the wounded to surgical care aboard ship often took more than three days.21
Regardless of these potential difficulties, the wounded must be rapidly evacuated to a facility that can provide the appropriate care for their injuries to ensure the best chance for survival. As mass casualty situations will be the norm during LSCO, the current medical evacuation (medevac) force structure is inadequate to meet the demand.22 Within the U.S. military, only the Army has dedicated ground and air ambulance evacuation capabilities. These capabilities include a medic who may provide essential lifesaving interventions during evacuation; however, but these resources are limited.
Currently, only one air ambulance (AA) company is assigned per division. This equates to 15 helicopters which will not simultaneously be ready to launch (RTL) due to maintenance and crew rest requirements.23 Additionally, while each AA can technically evacuate six litter patients, the current practice sees no more than two litter patients per platform per lift.24 Severely injured casualties often need multiple life-saving interventions en route. In this scenario, space constraints make carrying more than two casualties impractical. The transport of six patients is limited to the medically stable, who are transferred from one treatment facility to another and require little or no intervention. The evacuation of no more than two casualties in one lift translates to a maximum of 30 casualties per AA company over a given number of missions when all aircraft is available, which is an unlikely scenario. A number of variables, such as the length and difficulty of the mission, the need for crew rest, and maintenance requirements, impact the number of missions that can be flown daily.25 These variables make determining the exact number of evacuations an AA company can perform in 24 hours challenging; regardless, the number is unlikely to meet the demand.
Given these constraints, ground assets will be the primary avenue for casualty evacuation from the POI, Role 1 facilities, and casualty collection points (CCP). Ground evacuation during LSCO will also be challenged due to a limited number of dedicated ground ambulance (GA) platforms as well as distance, terrain, and potentially contested evacuation routes. Ground ambulances must be supplemented by non-standard casualty evacuation platforms (CASEVAC) without the capability of en route medical care.26 Studies have shown that medical care during evacuation also confers a survival benefit; therefore, casualties not receiving this care have a greater need for prompt evacuation to a medical facility.27 For these reasons, Role 2 medical facilities should be positioned forward in the brigade area near the FLOT to reduce the time and distance to treatment.
Properly positioned Role 2s will allow Role 1 aid stations to quickly evacuate casualties, allowing them to displace to continue supporting their assigned maneuver units. Studies of casualties sustained during GWOT have shown that evacuation to a treatment facility within 60 minutes decreases mortality.28 Failure to move Role 2 assets forward will mean increased evacuation times, leading to increased morbidity and mortality. Further, failure to provide these assets will make clearing Role 1 facilities challenging, presenting the combat commander with a difficult decision: move forward without medical assets, prolonging lines of communication, or forfeiting the initiative, losing operational momentum. Additional impacts of such a decision could mean further loss of life from a lack of adequate casualty care or ceding the combat advantage to the adversary.
Save Lives
In addition to facilitating the clearing of the battlefield to enable maneuver, placing a properly configured Role 2 medical facility in the brigade area close to the FLOT will save lives by providing far-forward surgical care and more advanced trauma resuscitation. However, this may only happen if Role 2 provides surgical care. Current U.S. medical doctrine is inconsistent with the requirement that Role 2 facilities provide surgical capability.29 Each branch of the U.S. military currently has different configurations for Role 2 facilities, as shown in Figure 1. As an example, Role 2 Medical capabilities for the Marine Corps include the Forward Resuscitative Surgery System (FRSS), Shock Trauma Platoon (STP), and a Surgical Company(SC).30 The FRSS provides mobile surgical capability near the FLOT but no patient-holding, while the STP provides patient-holding and advanced trauma resuscitation but no surgical capabilities.31 The SC provides surgical care, patient-hold, and advanced trauma resuscitation to support a Marine Corps Regiment.xxxiiArmy Role 2 capabilities include Forward Surgical Teams (FST); Forward Surgical and Resuscitation Detachments (FSRD), which are similar to the Marine FRSS; Medical Company Area Support (MCAS); and Brigade Support Medical Company (BSMC).33 Unlike the Marine Corps, the Army Role 2 medical company does not have surgical capability unless augmented by an FST or FSRD.34 To complicate the employment of the FST or FSRD, they are assigned to a Medical Command or Medical Brigade but are operationally controlled by a Role 3 medical facility.35 The Army has inconsistently applied the use of this surgical capability at Role 2, occasionally placing an FST or FSRD with a BSMC or MCAS while also using them independently even farther forward near the point of injury.
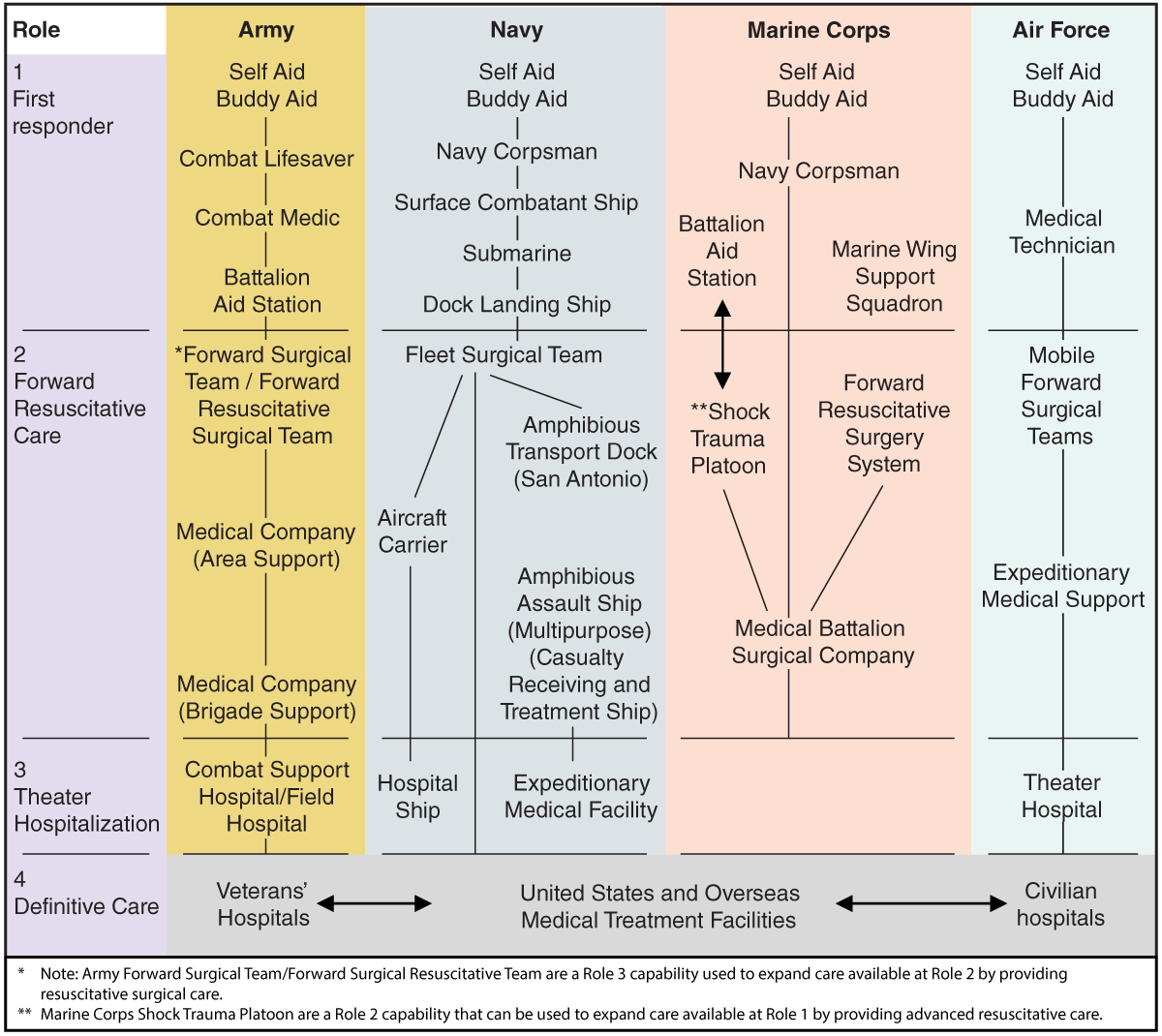
Fig. 1. Comparison of Role 2 configurations across the services, JP 4-02 Joint Health Services.xxxvi
The limitation of both the Marine Corps and Army forward surgical teams is patient-holding capability. Without an attached Role 2 holding facility, neither can hold more than eight patients for more than six hours.37 Surgery capability near the FLOT without patient-holding presents the same evacuation issues as a Role 1, limiting the effectiveness of forward surgical teams to clear the battlefield of casualties. During the GWOT, Secretary Robert Gates instituted the Golden Hour Policy to reduce the time for evacuation of casualties from the call for medevac to surgical care to 60 minutes.38 This policy helped reduce the case fatality rate during the GWOT from 13.7 percent before implementation to 7.6 percent.39 Requiring co-location of surgical teams with Role 2 medical facilities will reduce the time from initial injury to surgical intervention. This will allow life-saving care to remain within Golden Hour distance with the benefit of patient hold and robust trauma resuscitation with blood products, another intervention shown to help reduce combat deaths.40 Configuring Role 2 care in this way will improve survival and reduce the load on the medevac system.
With surgery and patient-holding closer to the FLOT, more AAs will be available to move casualties needing specialized surgical care to Role 3. Casualties who need surgical intervention but not specialty care can be evacuated via ground to a surgery-capable Role 2. There, they may have additional resuscitation and surgical intervention and be held forward while they recover. Requiring co-location of an FST or FRSD with a Role 2 eliminates two problems: how to provide urgent surgical care during LSCO in a contested battle space and how to care for those patients after surgical intervention. With Role 2 and surgical capabilities combined, these patients may be held for up to 72 hours before being returned to duty with their unit or evacuated to a higher level of care for further treatment.41 The ability to provide both forward surgical care and hold patients will decrease the burden on the evacuation system and should be the standard for military medicine at Role 2.
"In war, there is always a risk; however, the greater risk is not in placing medical assets forward but in failing to do so."
Regenerate Combat Power
Providing forward surgical capability and patient hold near the FLOT also helps regenerate combat power. An Army Role 2 BSMC or MCAS can hold 20 or 40 casualties, respectively, for up to 72 hours.42 The Marine Corps SC can only hold 10 patients.43 Many casualties will recover sufficiently from injuries to return to duty (RTD) within this time. Between January 2007 and March 2020, the RTD rate among combat casualties in the GWOT was 37.9 percent. Of the 10,182 casualties sustained, 3,856 returned to their units within 72 hours.44 This is the equivalent of four to five brigades worth of personnel.45 With an all-volunteer force, combat operations will likely be constrained by a lack of personnel and replacements for those no longer fit for the fight.46 In LSCO, where a force of 100,000 could sustain 50,000 casualties in one week, conserving the fighting strength is paramount to retaining combat power. A key to this effort is keeping those able to RTD as far forward as possible. The extended operational distances, rugged terrain, and contested air and ground LOC that make evacuation of casualties difficult will also impair their return to the FLOT when recovered. Returning service members to the fight from the Division or Corps area requires space on transport vehicles that could be used for critical sustainment items needed at the FLOT, such as fuel, parts, ammo, and food. Keeping those likely to RTD forward reduces the strain on the evacuation system and logistics trains and provides for the timely regeneration of combat power by reducing the time it takes to get service members back in the fight.
The Risk
There is inherent risk in placing surgical and Role 2 hold capabilities together nearer to the FLOT. The concern centers around the potential for losing high-skill, low-density military specialties such as surgery and anesthesiology if the adversary targets those facilities. Surgeons, anesthesiologists, and other medical professionals require years of training and are not easily replaced. Though protected by the Geneva Conventions from deliberate targeting, there is an admitted risk of injury or death to medical personnel placed forward to care for the wounded.47 In WW2, during the battle for Saipan, the medical section for the 1st battalion, 29th Regiment, had 27 of their 40 personnel wounded, including two of their medical officers, who, despite their wounds, continued to work until they could be relieved.48 In the European theater, during the invasion of Anzio in 1944, the 95th Evacuation Hospital was bombed, killing six patients, three nurses, and two physicians.49 In 2011, an army nurse was killed by a sniper in Afghanistan.50 In war, there is always a risk; however, the greater risk is not in placing medical assets forward but in failing to do so.
After the Golden Hour Policy implementation, the case fatality rate in the GWOT decreased by four percent.51 Extrapolated over 50,000 casualties equals 2,000 lives that could be saved with early intervention. This number is just shy of a Marine Corps regiment.52 The lifesaving potential of forward-placed medical assets outweighs the risk of harm. Further, the U.S. military has placed surgical teams forward on the battlefield in the past; hence, the “Forward Surgical Team” moniker. The unit is designed to be set forward to provide surgical capabilities to save lives. Role 2 units with patient-holding capabilities are designed to be forward in the Brigade Support Area or equivalent. They provide advanced trauma resuscitation and patient-hold capabilities unavailable at Role 1. Combining the surgical capabilities of an FST or FSRD with the advanced trauma resuscitation and patient-hold capabilities of a BSMC or MCAS provides the best chance to save lives and regenerate combat power.

Soldiers at Fort Carson, Colorado, ... [become] the first active duty unit to set up and test the field hospital -- Army Medicine’s modernized, modular update to the well-known Combat Support Hospital. (Photo Credit: U.S. Army)
Another option frequently asserted maintains that the focus should be on prolonged casualty care (PCC) at Role 1 because of the danger of losing highly skilled military specialties. The assertion holds that doing so will mitigate evacuation difficulties, allowing for robust stabilization and treatment until casualties can be evacuated while avoiding the risk of losing skilled medical professionals. However, the argument overlooks the need for Role 1 facilities to remain mobile to support the maneuver units to which they are assigned. PCC is defined as “patient care for extended periods of time.”53 It includes not only initial life-saving trauma resuscitation but the creation of “nursing care plans” and a “wake, rest, chow plan.”54 This level of care, especially for multiple casualties, would make mobility of Role 1 challenging at best and impossible at worst. This is not to denigrate the concept of prolonged casualty care but to point out that it is antithetical to maintaining mobility for Role 1 and best performed at a Role 2 purposely suited for the task. To continue to support the maneuver unit, Role 1 care should focus on initial stabilization and evacuation to the next level of care.
Finally, the medical officers’ duty within the U.S. military is to save the fighting strength. Joining the military comes with the inherent danger of war, regardless of military occupation. This is not to suggest that risks should not be considered when placing medical assets forward. Rather, medical officers have a duty and moral obligation to take calculated risks to save the lives of those in close combat with the adversary. To join the military with the hope of avoiding danger is disingenuous. Under the Geneva Conventions, medical team members are afforded protected status designed to prevent them from being targeted during war.55 This does not mean, however, that all danger will be avoided while saving lives. Instead, the medical corps should take prudent risks to do its duty, caring for those fighting on the frontlines.
Conclusion
Twenty years of the GWOT have conditioned the U.S. Military and public to exceptionally low casualties and a survival rate greater than 90 percent.56 This experience has ill-prepared the U.S. for war under the conditions of large- scale combat operations. A fight with a near-peer adversary will incur casualties to U.S. forces not seen since WW2. Warfighter simulations show casualty rates in LSCO of more than 50% percent.57 If these rates prove true, they will strain combat power, medical evacuation, and treatment. War in the Pacific will compound the strain with its scattered island chains, jungle terrain, and prolonged SLOC. In LSCO, gone are the days of fighting from fixed forward operating bases, with air superiority and medical assets operating safely behind barriers of concrete and sand. Maneuver units must move to survive, seize the initiative, and defeat the adversary. So, too, will the medical assets that sustain them.
Role 1 medical facilities need to be able to advance on the battlefield unencumbered by casualties. To enable this, casualties need to be stabilized and quickly evacuated. Those requiring surgery should be treated as far forward as possible to save the most lives. It is time to rethink how medical assets are allocated on the battlefield, requiring the co-location of a surgical team with a Role 2 facility near the FLOT. This provides the best chance to achieve care in the Golden Hour to save lives, clear the battlefield of casualties, and return service members to units quickly to regenerate combat power. There is risk in placing medical assets closer to the fight despite protections provided by the Geneva Conventions. Medical personnel and equipment could be lost, but there is a guaranteed loss of lives and combat power if that prudent risk is not taken. It is time to require Role 2 facilities to have surgical capabilities. The INDOPACOM commander should require the placement of these medical assets together forward on the battlefield to conserve the fighting strength.
Bibliography
“Army Capt Joshua M. McClimans.” Honor the Fallen., accessed 26 Sept, 2023, https://thefallen.militarytimes.com/ar-my-capt-joshua-m-mcclimans/6348288.
“Conflict Casualties.” Defense Casualty Analysis System., last modified 22 Sept, accessed 22 Sept, 2023, https://dcas.dmdc.osd.mil/dcas/app/conflictCasualties/oco/summary/reason.
Department of the Army. Flight Regulations AR 95-1. Washington DC: Department of the Army, 2018. https://armypubs.army.mil/epubs/DR_pubs/DR_a/pdf/web/ARN5966_AR_95-1_WEB_FINAL.pdf.
Department of the Army. Army Health System, FM 4-02 C1. Washington DC: Department of the Army, 2022. https://armypubs.army.mil/epubs/DR_pubs/DR_a/ARN35791-FM_4-02-001-WEB-3.pdf.
Department of the Army. Casualty Evacuation, ATP 4-02.13. Washington DC: Department of the Army, 2021. https://armypubs.army.mil/epubs/DR_pubs/DR_a/ARN32888-ATP_4-02.13-000-WEB-1.pdf
Department of the Army. Medical Evacuation, ATP 4-02.2. Washington DC: Department of the Army, 2019. https://armypubs.army.mil/epubs/DR_pubs/DR_a/pdf/web/ARN17834_ATP%204-02x2%20FINAL%20WEB.pdf.
Department of the Army. The Medical Detachment, Forward Resuscitative and Surgical, ATP 4-02.25. Washington DC: Department of the Army, 2020. https://armypubs.army.mil/epubs/DR_pubs/DR_a/ARN37250-ATP_4-02.25-001-WEB-2.pdf.
Department of the Army. The Medical Company (Role 2) ATP 4-02.6. Washington DC: Department of the Army, 2022. https://armypubs.army.mil/epubs/DR_pubs/DR_a/ARN36760-ATP_4-02.6-000-WEB-1.pdf.
Geneva Convention of 1949 for the Amelioration of the Sick and Wounded in the Armed Forces in the Field, Public Law article 19-24, (1949). https://www.icrc.org/en/doc/assets/files/publications/icrc-002-0173.pdf.
Department of the Navy. Health Service Support Reference Guide, U.S. Marine Corps MCRP 3-40A.5. Washington, DC: Department of the Navy, Headquarters United States Marine Corps, 2018. https://www.marines.mil/Portals/1/Publications/MCRP%203-40A.5.pdf?ver=2019-03-12-145532-823.
Joint Chiefs of Staff. Joint Health Services, JP 4-02. Washington, DC: Joint Chiefs of Staff, 2017. https://www.jcs.mil/Portals/36/Documents/Doctrine/pubs/jp4_02ch1.pdf?ver=2018-10-10-113551-603.
“Military Units.” U.S. Department of Defense., accessed 26 Sept, 2023, https://www.defense.gov/Multimedia/Experience/Military-Units/Army/#other-units.
“Prolonged Casualty Care Guidelines.” Joint Trauma System., accessed 26 Sept, 2023, https://jts.health.mil/assets/docs/cpgs/prolonged_casualty_care_guidelines_21_dec_2021_id91.pdf.
Department of the Army. Technical Manual Operators Manual for Helicopters, Utility Tactical Transport UH-60M, HH60M. TM 1-1520-280-10. Washington DC: Department of the Army, 2023. https://armypubs.army.mil/Product-Maps/PubForm/Details.aspx?PUB_ID=1027003.
War Department. Medical Field Manual: Medical Service of Field Units, FM8-10 (Washington DC: War Department, 1942) 1942.
April, Michael D., Rachel E. Bridwell, Jessica Jones, Joshua Oliver, Brit Long, and Steven G. Schauer. 2022. “Descriptive Analysis of Casualties Rapidly Returned to the Fight After Injury: Reverse Triage Implications for Large Scale Combat Operations.” Medical Journal, US Army Medical Center of Excellence (MEDCoE): 3-9. https://search.ebscohost.com/login.aspx?direct=true&db=tsh&AN=156208389&site=ehostlive.
April, Michael D., Peter J. Stednick, and Nicholas B. Christian. 2021. “A Descriptive Analysis of Notional Casualties Sustained at the Joint Readiness Training Center: Implications for Health Service Support during Large-Scale Combat Operations.” Medical Journal, US Army Medical Center of Excellence (MEDCoE): 3-8. https://search.ebscohost.com/login.aspx?direct=true&db=tsh&AN=152354384&site=ehostlive.
Barno, David, Bensahel, Nora. “Three Things the Army Chief of Staff Wants You to Know.”
War on the Rocks., last modified -05-23T07:55:27+00:00, accessed Sep 16, 2023, https://warontherocks.com/2017/05/three-things-the-army-chief-of-staff-wants-you-toknow/.
Barr, Justin, Kenneth J. Cherry, and Norman M. Rich. 2019. “Vascular Surgery in the Pacific Theaters of WWII: The Persistence of Ligation Amid Unique Military Medical Conditions.”
Annals of Surgery 269 (6): 1054-1058. https://doi.org/10.1097/sla.0000000000002849.
Cancian, Mark F., Cancian, Matthew, Heginbotham, Eric. 2023. 230109_Cancian_FirstBattle_NextWar.Pdf. https://csis-websiteprod.s3.amazonaws.com/s3fs16public/publication/230109_Cancian_FirstBattle_NextWar.pdf?VersionId=WdEUwJYWIySMPIr3ivhFolxC_gZQuSOQ.
Fandre, Matthew. 2020. “Medical Changes Needed for Large-Scale Combat Operations: Observations from Mission Command Training Program Warfighter Exercises.” Military Review 100 (3): 36-45. https://search.ebscohost.com/login.aspx?direct=true&db=mth&AN=143353622&site=ehostlive.
Gates, Robert Michael. 2014. Duty: Memoirs of a Secretary at War. New York: Alfred A. Knopf.
Hughey, Scott, Jacob Cole, Adam Brust, Kyle Checchi, and Andrew Lin. “Surgical Casualty Care in Contested Distributed Maritime Operations: Lessons Learned from the Falklands War.” Military Medicine 00, (2023): 1-5.
Jackson, D. S., C. G. Batty, J. M. Ryan, and W. S. McGregor. 1983. “The Falklands War: Army Field Surgical Experience.” Annals of the Royal College of Surgeons of England 65 (5): 281-285. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2494365/.
Kotwal, Russ S., Jeffrey T. Howard, Jean A. Orman, Bruce W. Tarpey, Jeffrey A. Bailey, Howard R. Champion, Robert L. Mabry, John B. Holcomb, and Kirby R. Gross. 2016. “The Effect of a Golden Hour Policy on the Morbidity and Mortality of Combat Casualties.” JAMA Surgery 151 (1): 1-10. doi:10.1001/jamasurg.2015.3104. http://dx.doi.org/10.1001/jamasurg.2015.3104.
Schwartz, Joseph L. 1953. THE HISTORY OF THE MEDICAL DEPARTMENT OF THE UNITED STATES NAVY IN WORLD WAR
II Volume 1: A Narrative and Pictorial Volume. U.S. Navy Bureau of Medicine and Surgery Office of Medical History Collection. https://archive.org/details/HistoryOfTheMedicalDeptInWWIIV1
Wiltse, Charles M. 1987. Medical Service in the Mediterranean and Minor Theaters. https://history.army.mil/html/books/010/10-8/index.html
Notes
1. Conflict Casualties.” Defense Casualty Analysis System, September 22, 2023. https://dcas.dmdc.osd.mil/dcas/app/conflictCasualties.
2. Russ S. Kotwal et al., “The Effect of a Golden Hour Policy on the Morbidity and Mortality of Combat Casualties,” JAMA Surgery 151, no. 1 (2016): 15, https://doi.org/10.1001/jamasurg.2015.3104: 22.
3. Matthew Fandre, “Medical Changes Needed for Large-Scale Combat Operations: Observations from Mission Command Training Program Warfighter Exercises.” Military Review 100 (3)2020: 37. https://search.ebscohost.com/login. aspx?direct=true&db=mth&AN=143353622&site=ehost-live.
4. Mark F Cancian, Matthew Cancian, Eric Heginbotham. 2023. 230109_Cancian_FirstBattle_NextWar.Pdf. https://csis- website-prod.s3.amazonaws.com/s3fspublic/publication/230109_Cancian_FirstBattle_NextWar.pdf?VersionId=W- dEUwJYWIySMPIr3ivhFolxC_gZQuSOQ.: 120.
5. Joseph L Schwartz, “The History of the Medical Department of the United States Navy in World War II Volume 1: A Narrative and Pictorial Volume: U.S. Navy. Bureau of Medicine and Surgery: Internet Archive, January 1, 1970, https://archive.org/details/HistoryOfTheMedicalDeptInWWIIV1: 93.
6. Schwartz, “The History of the Medical Department” 104
7. David Barno, Nora Bensahal, “Three Things the Army Chief of Staff Wants You to Know.” War on the Rocks., last modified -05-23T07:55:27+00:00, accessed Sep 16, 2023, https://warontherocks.com/2017/05/three-things-thearmy-chief-of-staff-wants-you-to-know/.
8. Levels of medical care in the U.S. military are defined as Roles. Role 1 is first aid, triage, resuscitation, and stabiliza- tion. Role 2 provides advanced trauma management, including the continuation of resuscitation from role 1 and may include damage control surgery, but it is not required. Theater hospitalization, or Role 3, is the only level of a theater treatment facility that, by doctrine, is required to provide surgical care. Role 3 is typically located in the Division or equivalent area JP 4-05, II2-3.
9. Kotwal, “The Effect of a Golden Hour Policy,” 22
10. Joint Chiefs of Staff, Joint Health Services, JP 4-02 (Washington D.C.: Joint Chiefs of Staff 2017), II-2, https://www.jcs.mil/Portals/36/Documents/Doctrine/pubs/jp4_02ch1.pdf?ver=2018-10-10-113551-603.
11. Department of the Navy, Health Service Support Reference Guide, U.S. Marine Corps, MCRP 3-40A.5 (Washington D.C.: Department of the Navy, Headquarters United States Marine Corps 2018), 1-6,1-7, https://www.marines.mil/Portals/1/Publications/MCRP%203-40A.5.pdf?ver=2019-03-12-145532-823; Joint Chiefs of Staff, Joint Health Ser- vices,II-1.
12. Joint Chiefs of Staff, Joint Health Services, JP 4-02 II2-3.
13. Joint Chiefs of Staff, Joint Health Services, JP 4-02 II3.
14. Department of the Army, Army Health System, FM 4-02 C1 (Washington DC: Department of the Army, 2022), A-5, https://armypubs.army.mil/epubs/DR_pubs/DR_a/ARN35791-FM_4-02-001-WEB-3.pdf.
15. Department of the Army, Army Health System, FM 4-02, A-4.
16. D. S. Jackson, et al., “The Falklands War: Army Field Surgical Experience.” Annals of the Royal College of Surgeons of England 65 (5): (1983):281, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2494365/.
17. Jackson et al., “The Falklands War: Army Field Surgical Experience,” 281.284
18. Jackson et al., “The Falklands War: Army Field Surgical Experience,” 282,283
19. Scott Hughey, et al., “Surgical Casualty Care in Contested Distributed Maritime Operations” Military Medicine 100, (2023): 2. https://academic.oup.com/milmed/advance-article/doi/10.1093/milmed/usad304/7237340.
20. Jackson et al., “The Falklands War,” 284
21. Schwartz, “The History of the Medical Department”,173
22. Justin Barr, Kenneth J. Cherry, and Norman M. Rich. “Vascular Surgery in the Pacific Theaters of World War II: The Persistence of Ligation Amid Unique Military Medical Conditions.” Annals of Surgery 269, no. 6 (June 2019): 1056. https://doi.org/10.1097/sla.0000000000002849.
23. Mass casualty situation is considered any number of human casualties that exceed available medical support capa- bilities JP4-02
24. Due to safety issues, aviation crews are limited to how many hours they can fly per day. See AR95-1 and the Army Safety Center Leaders Guide to Soldier and Crew Endurance for additional details at https://safety.army.mil/ LinkClick.aspx?fileticket=Qnw_bNDJ-nE=; Department of the Army, Medical Evacuation, ATP 4-02.2 (Washington DC: Department of the Army, 2019), 3-6, https://armypubs.army.mil/epubs/DR_pubs/DR_a/pdf/web/ARN17834_ATP%2042x2%20FINAL%20WEB.pdf.
25. Department of the Army, Technical Manual Operators Manual for Helicopters, Utility Tactical Transport UH-60M, HH60M. TM 1-1520-280-10 (Washington DC: Department of the Army, 2023), 4-86, https://armypubs.army.mil/ProductMaps/PubForm/Details.aspx?PUB_ID=1027003
26. Department of the Army, Flight Regulations, AR95-1 (Washington D.C., 2018), 10, https://armypubs.army.mil/epubs/DR_pubs/DR_a/pdf/web/ARN5966_AR_95-1_WEB_FINAL.pdf.
27. Department of the Army, Casualty Evacuation, ATP 4-02.13 (Washington DC: Department of the Army2021), 1-1, https://armypubs.army.mil/epubs/DR_pubs/DR_a/ARN32888-ATP_4-02.13-000-WEB-1.pdf.
28. Kotwal et al., Effect of a Golden Hour, 16
29. Kotwal et al., Effect of a Golden Hour, 22
30. Joint Chiefs of Staff, Joint Health Services, JP 4-02 II2-3.
31. Department of the Navy, Health Service Support Reference Guide, U.S. Marine Corps, MCRP 3-40A.5 (Washington D.C.: Department of the Navy, Headquarters United States Marine Corps 2018), 1-6,1-7, https://www.marines.mil/Portals/1/Publications/MCRP%203-40A.5.pdf?ver=2019-03-12-145532-823; Joint Chiefs of Staff, Joint Health Ser- vices,II-2, II-3.
32. Department of the Navy, Health Service Support Reference Guide, 1-6.
33. Department of the Navy, Health Service Support Reference Guide, 1-7.
34. Department of the Army, Army Health System, 1-12.
35. Department of the Army, Army Health System, 1-12. https://armypubs.army.mil/epubs/DR_pubs/DR_a/ARN35791-FM_4-02-001-WEB-3.pdf
36. Department of the Army, The Medical Detachment, Forward Resuscitative and Surgical, ATP 4-02.25 (Washington DC: Department of the Army 2020), 1-1, https://armypubs.army.mil/epubs/DR_pubs/DR_a/ARN37250-ATP_4-02.25-001-WEB-2.pdf.
37. Joint Chiefs of Staff, Joint Health Services,II-4.
38. Department of the Navy, Health Service Support Reference Guide, 2-17.
39. Robert Michael Gates, Duty: Memoirs of a Secretary at War (New York: Alfred A. Knopf, 2014), 304-305
40. Russ S. Kotwal et al., “The Effect of a Golden Hour Policy on the Morbidity and Mortality of Combat Casualties,” JAMA Surgery 151, no. 1 (2016): 17,18, http://dx.doi.org/10.1001/jamasurg.2015.3104.
41. Department of the Army, Army Health System, 1-12; Kotwal, Effect of a Golden Hour, 22.
42. Department of the Army, the Medical Company (Role 2) ATP4-02.6 (Washington D.C.: Department of the Army, 2022) 2-2,2-5, https://armypubs.army.mil/epubs/DR_pubs/DR_a/ARN36760-ATP_4-02.6-000-WEB-1.pdf.
43. Department of the Army, The Medical Company (Role 2), 2-2, 2-5.
44. Department of the Navy, “Health Service Support Reference Guide,” 2-16.
45. Michael D. April, et al., 2022. “Descriptive Analysis of Casualties Rapidly Returned to the Fight After Injury: Reverse Triage Implications for Large Scale Combat Operations.” Medical Journal, US Army Medical Center of Excellence (MEDCoE),(2022): 3, https://search.ebscohost.com/login.aspx?direct=true&db=tsh&AN=156208389&site=e-host-live.
46. “Military Units.” U.S. Department of Defense., accessed 26 Sept, 2023, https://www.defense.gov/Multimedia/Expe-rience/Military-Units/Army/#other-units.
47. April, Analysis of Casualties Returned to the Fight, 5.
48. Geneva Convention of 1949 for the Amelioration of the Sick and Wounded in the Armed Forces in the Field, Public Law article 19-24, (1949), 43,44.
49. Schwartz, “The History of the Medical Department,” 180.
50. Charles M Wiltse, “Medical Service in the Mediterranean and Minor Theaters,” 275, https://history.army.mil/html/ books/010/10-8/index.html.
51. “Army Capt. Joshua M. McClimans.” Honor the Fallen., accessed 26 Sept 2023, https://thefallen.militarytimes.com/ army-capt-joshua-m-mcclimans/6348288.
52. Kotwal, Effect of a Golden Hour, 15.
53. “Military Units.” U.S. Department of Defense.
54. “Prolonged Casualty Care Guidelines.” Joint Trauma System., accessed 26 Sept 2023, 5,7 https://jts.health.mil/as- sets/docs/cpgs/prolonged_casualty_care_guidelines_21_dec_2021_id91.pdf.
55. “Prolonged Casualty Care”.
56. Geneva Convention of 1949, 43,44.
57. “Conflict Casualties.” Defense Casualty Analysis System.
Author
COL Patricia “Trish” Brown graduated with distinction from the United States Naval War College in 2024. She currently serves as the Army Medical Department branch manager for the Utah Army National Guard and previously served as the Deputy Commander for Clinical Services for the Utah Medical Readiness Command. COL Brown has also served tours in Afghanistan as an Aviation Physician Assistant and in Iraq and Kuwait as a Brigade PA. In her civilian career, she has practiced emergency medicine since 2009 and is an experienced hospitalist and surgical PA.